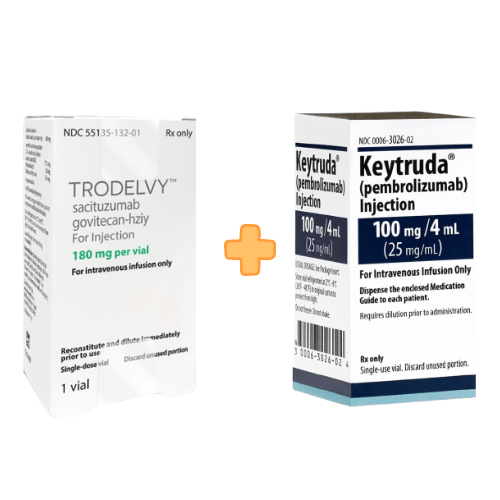
Gilead’s Sciences announced the promising activity of Trodelvy (sacituzumab govitecan-hziy) in combination with Merck’s Keytruda (pembrolizumab) on the basis of results from a global, open-label, phase-2 EVOKE-02 trial (https://clinicaltrials.gov/study/NCT05186974.) with or without platinum agents in previously untreated metastatic non-small cell lung cancer (NSCLC) without genomic alterations.
NSCLC is a type of lung cancer that is most common and accounts for up to 85% of diagnoses.
Trodelvy is a first-in-class trop-2-directed antibody-drug conjugate. Trop-2 is highly expressed in several tumor types on cell surface antigens. It is approved in the U.S. and the European Union for the treatment of certain patients with pre-treated HR+/HER2- metastatic breast cancer.
The preliminary analysis of the study includes the results of two cohorts:
Trodelvy in combination with KEYTRUDA in first-line metastatic squamous/non-squamous NSCLC with PD-L1 tumor proportion score (TPS) ≥ 50% (Cohort A) and TPS < 50% (Cohort B).
- In Cohort A (n=29), the confirmed and unconfirmed objective response rate (ORR) was 69%, and the disease control rate (DCR) was 86%.
- In Cohort B (n=32), confirmed and unconfirmed ORR was 44%, and DCR was 78%.
Across both cohorts, the ORR was 56%, and DCR was 82%. The median duration of response (DoR) was not reached at the time of data cut-off, and the DoR rate at six months was 88% in both cohorts.
The primary endpoints are objective response rate (ORR) which is assessed by independent review per Response Evaluation Criteria in Solid Tumors (RECIST 1.1) and the percentage of participants experiencing dose-limiting toxicities (DLTs) per dose level in the safety run-in cohorts. Some additional efficacy measures include:
- Progression-free survival (PFS)
- Overall survival (OS)
- Duration of response (DoR)
- Disease control rate (DCR)
The safety profile of Trodelvy in combination with KEYTRUDA was consistent and the treatment-emergent adverse events (TEAEs) were diarrhea (54%), anemia (48%), and asthenia (38%). The discontinuation rate due to AEs was 18%. One treatment related death was observed due to sepsis.
The positive response rates and DoR across patients treated with this combination show positive results compared to anti-PD1 monotherapy treatment. These results were encouraging as worldwide, more than two million people were diagnosed with lung cancer in 2020 and NSCLC is the most common type of lung cancer, accounting for up to 85% of diagnoses. Results support further investigation of this combination in first-line treatment of metastatic NSCLC.
The results of this trial were presented to the International Association for the Study of Lung Cancer (IASLC) 2023 World Conference on Lung Cancer.



